As a goal for 2019, I want to try and share a few more personal blog posts with all of you. As much as I love showcasing all of our fun activities, craft projects, favorite recipes, and all of the stories that we love to read…our family life and parenting journey obviously includes a whole lot more. To kick off the new year, I shared an emotional post all about My Breastfeeding Battle. And today, I wanted to delve into a new topic – Our Experience with Pediatric Asthma.
As many of you know, asthma is a chronic lung disease that inflames and narrows the airways, making it difficult to move air into and out of your lungs. The condition can cause recurring periods of wheezing, chest tightness, shortness of breath, and coughing. According to the Centers for Disease Control and Prevention (CDC) roughly 1 in 12 people in the United States has asthma. And it is the most common chronic condition among children. In a 2017 Summary of U.S. Health Statistics, the CDC reported that 6.2 million children under the age of 18 have asthma. And that number continues to grow every year.
When a child has asthma, their lungs become extremely sensitive to certain triggers – ranging from respiratory infections and colds, allergens, air pollution, cigarette smoke, exercise, and more. Sadly, asthma can be a life-threatening disease if it is not properly managed. Statistics show that in 2016, there were 3,651 deaths attributed to asthma, although asthma-related deaths are rare among children.
I happen to be very familiar with pediatric asthma, because I myself was diagnosed with asthma as a child. I remember countless nights of coughing, a variety of different inhalers and asthma medications, numerous doctor’s visits, and a few hospital stays. My asthma was mostly allergy-related. As a result, there was an effort to build my immunity against various allergens. For longer than I care to remember, I would visit the doctor’s office every Saturday morning to receive an injection of a particular allergen (in a small dose). My mom and I would then sit and wait to see if I had any type of allergic reaction. I had to have an allergy shot every single week – even if we were out of town or on vacation. I can’t recall exactly how long this routine lasted, I just remember it coming to an end after one particular injection caused my arm to redden and swell.
I’m also fully aware that asthma is a genetic disease and one that it is extremely likely to be passed down to future generations. When I became pregnant, I crossed my fingers that our little nugget would be blessed with her father’s (asthma-free) genetics. But as luck would have it, she has been graced with a pediatric asthma diagnosis as well. And I’m also now aware that doctors are hesitant to diagnose asthma in a child that is under two years of age. Needless to say, our daughter’s first two years of life were a bit of a struggle when it came to respiratory infections.

Anytime our daughter would pick up a common cold, it would very quickly escalate into never-ending coughing fits – that were notably worse at night. Our sweet little girl would struggle to sleep. And my husband and I would do anything we could think of to try and help her. We would prop her up in bed, sit with her in the rocking chair, steam her in the bathroom, suck out the mucus from her nasal cavities…and when all else failed, we would buckle her into her car seat and drive her around for hours and hours each night (periodically allowing some cold night air to seep through the car windows, to ease her breathing). But she would still cough constantly…for days and days on end. It was excruciating, heartbreaking, and completely exhausting.
And this went on for two years. The winter and spring months were our absolute worst. Six month time-spans would go by in one sleepless blur. And she would occasionally get respiratory infections during the summer. 🙁 Needless to say, we made countless visits to our pediatrician’s office – most of which resulted in a Prednisone prescription (the only thing that seemed to help our daughter stop coughing and kick the illness). Between our daughter’s countless respiratory infections, and all of the early childhood checkups, it sometimes felt like we actually lived at the doctor’s office. In fact, numerous people (patients, nurses, doctors, etc.) have commented on how well-behaved, helpful, and compliant our daughter is during a doctor/hospital visit. And it’s because for the first years of her life, the doctor’s office was were she spent a large majority of her time.
Our absolute worst asthma experience (to-date) was when our little nugget was almost 1-1/2 years old. She came down with a cold (that she picked up at daycare) and we began going through our usual motions. She began coughing uncontrollably…she would often cough so hard it would cause her to vomit. When I noticed her breathing becoming more strained, we made a beeline for the doctor’s office. They placed a pulse oximeter on her index finger and discovered that her oxygen saturation level was at 86 – anything below 90 is a problem. And her poor little lungs…the skin between her ribs had started to suck inward every time she tried to inhale. We were immediately admitted to the hospital. At the time, they did what they call a quick (on-site) swab test for RSV. It came back negative. After a two-night stay, we were discharged.
Her coughing symptoms started to subside, but they never completely went away. And three weeks later, we were back in the hospital. They ran another quick swab test for RSV, but this time they decided to send a sample to Children’s Hospital as well. The on-site test came back negative again, but the sample that was sent to Children’s came back positive for RSV. Respiratory Syncytial Virus is a common respiratory virus, but one that can be extremely dangerous for infants and young children. According to the CDC, an estimated 57,000 children, younger than 5 years of age, are hospitalized due to an RSV infection every year in the United States. I had a feeling that our daughter had been suffering from RSV this entire time (since both of the hospital’s quick tests had come back negative). Needless to say, RSV was a battle for our little girl. I unfortunately picked it up after her, and I can say that even as an adult, it is by far and away the worst cold I’ve ever experienced. We made our way home from the hospital 4 days later.

It is extremely difficult to see your child hooked up to all sorts of tubes and machines…to watch them struggle and suffer when there is nothing that you can do to help them, except try your best to comfort them in any way that you can. After our repeat stints in the hospital, I was constantly on edge at the sound of our daughter’s cough or sneeze. We even purchased our own pulse oximeter from Walgreens…just so that we could keep a closer eye on our daughter’s oxygen saturation levels when she became sick in the future.
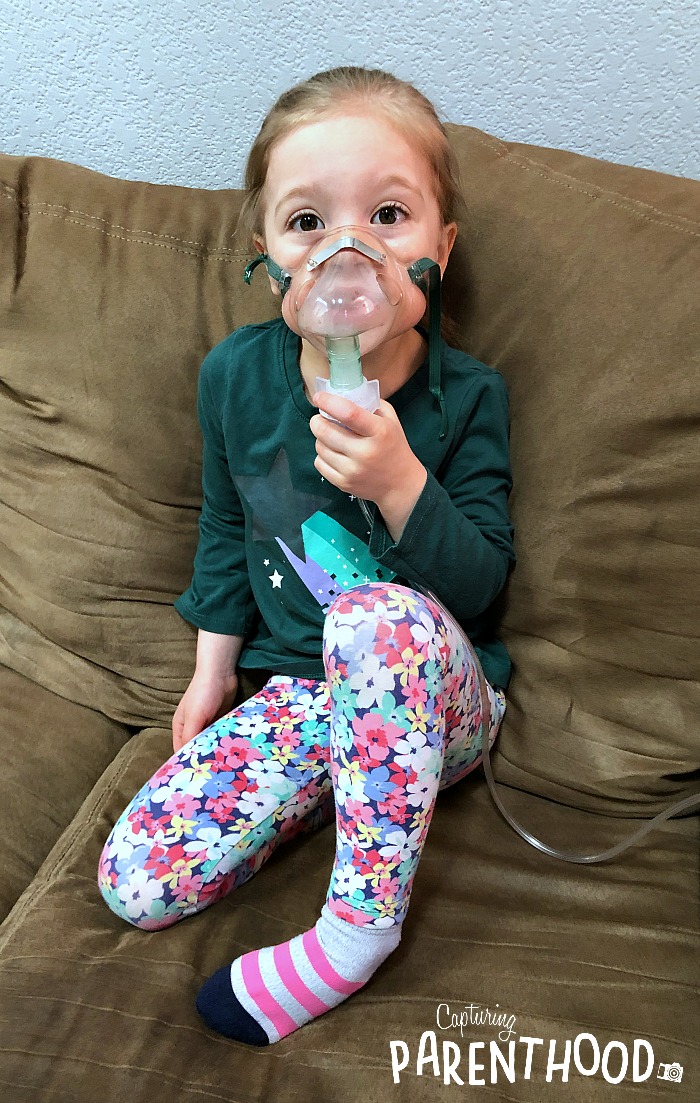
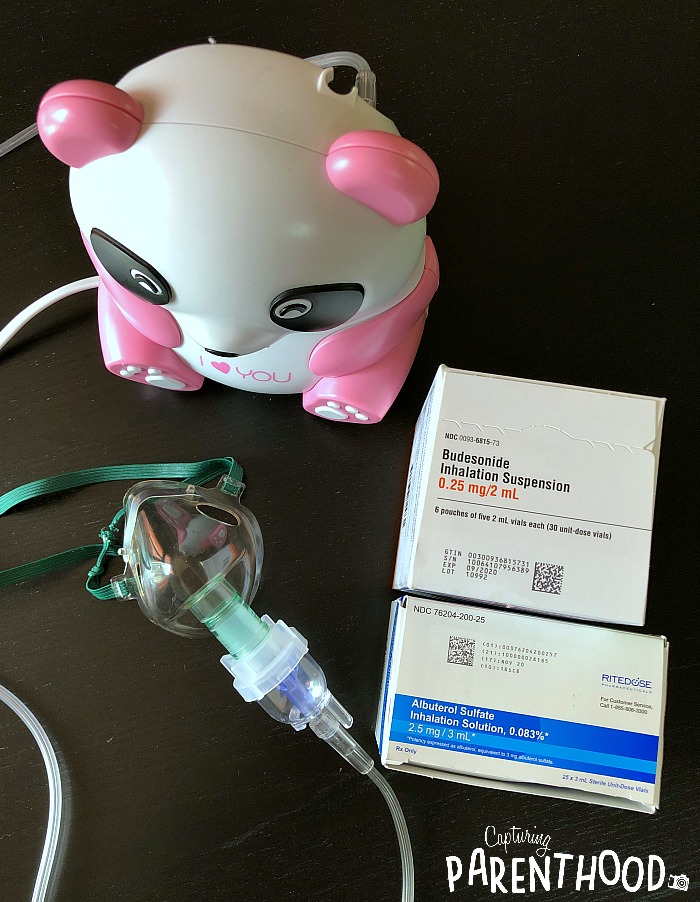
In the passing months, our daughter struggled with a few more respiratory viruses – all resulting in endless days and nights of coughing. During a mid-summer episode, it was recommended that we try a breathing treatment of Albuterol, given through a nebulizer. A nebulizer is a machine that changes medication from a liquid to a mist, so that it can be more easily inhaled into the lungs. We came home with a cute little panda nebulizer, that we named Daisy.
And upon getting sick again, three weeks after her second birthday, her pediatrician recommended that we pay a visit to a pediatric specialist at National Jewish Health – one of the nation’s leading respiratory hospitals.

At National Jewish, our daughter was tested for all of the top allergens. I was honestly expecting her to have several, since my asthma was allergy-induced. She tested negative for every single one – though we were informed that she could develop allergies at any point in the future. But for the time being, allergies are a non-issue. Based on her numerous experiences with respiratory viruses that resulted in the need for Prednisone doses, as well as her hospital stays…our daughter was officially diagnosed with asthma and prescribed a Flovent inhaler (an inhaled corticosteroid). Her asthma is strictly respiratory virus-induced. She only struggles when she has a cold.
We embarked on a twice-daily regimen of Flovent. We were also prescribed a ProAir (albuterol) inhaler, to use as necessary, when our daughter is battling a respiratory infection. Our little nugget was really great about her new medicine routine for the first few weeks – and then the novelty wore off. She was no longer interested in having to sit down for a breathing exercise every morning and evening. My husband and I had to brainstorm a new way to peak her interest every few weeks. We used sticker reward charts (that had come in handy during potty training), and yes…even bribery. 🙂 Eventually, she just accepted the new routine as part of life and she stopped fighting us when it came to doing her medicine.
Our daughter is now 4-1/2 years old. She went from the Flovent inhaler to the QVAR inhaler (due to an insurance change), and when the QVAR manufacturer decided to change their product (resulting in impossible use by young children), we were switched to a nebulized Budesonide prescription. Daisy, the panda nebulizer, now has a prominent spot in our living room. As the years have passed, the inhaled medications have made a drastic difference. The last time that we had to go to the doctor’s office was for our little nugget’s 4-year checkup! And when she gets a common cold, she can usually weather it with her daily Budesonide treatment, as well as the ProAir inhaler.
Our current goal is to try and take our daughter off of her daily nebulizer treatment starting this summer…to see what happens. Her pediatric specialist, at National Jewish, informed us that young children with this type of asthma tend to outgrow it around 4 to 5 years of age. Fingers crossed. I outgrew my asthma too, but at a much later age – around the start of middle school.
Now I must admit, I’m a bit hesitant to pull her off of the daily medication. If you had asked me last summer I would have been all for it, but we’ve had a pretty rough winter this year. Our daughter has been sick much of November, December, January, and February. And while we have stayed out of the doctor’s offices, and we have not had to resort to a Prednisone prescription, her coughing has been more reminiscent of her first two years of life. Just incessant throughout the entire night – better during the day – but absolutely no sleep. Our household has once again been running on fumes and it is incredibly exhausting. Lately, when she’s sick, we’ve had to double-up on the nebulized Budesonide, as well as switch over to nebulized Albuterol. So now I’m wondering, with the winter that she’s had, maybe it’s not such a great idea to take her off the medication just yet. But I guess we will figure that all out when we go in for our scheduled visit in a couple of months.
Right now, I’m just thankful that we were able to find a medication that helped ease our daughter’s struggle with respiratory viruses. Asthma is so common, but it can also be incredibly scary, as it affects an all-important life-giving function…breathing. And little ones suffering from asthma can be absolutely terrifying. So, here’s hoping that our daughter’s asthma symptoms subside in the next year or two.
Have any of your little ones been diagnosed with asthma? Feel free to share your experiences, struggles, and tips and tricks below in the comments. It’s always nice to know that we are not the only ones going through a not-so-pleasant part of parenthood. 🙂